Effective April 1, 2023, Phelps Health changed to a provider-based billing (PBB) system. Nearly all Phelps Health clinics will operate as provider-based clinics. Below are answers to frequently asked questions about PBB.
What is provider-based billing (PBB)?
Provider-based billing, or hospital-based outpatient billing, is a type of billing for services provided in a clinic or department that is considered part of the hospital. Clinics located miles away from the main hospital campus can be considered part of the hospital, as is the case with Phelps Health.
Patients benefit because all hospital outpatient departments are subject to additional stringent quality standards and are monitored by The Joint Commission, an independent, not-for-profit organization that accredits and certifies more than 21,000 healthcare organizations and programs in the United States.
What Phelps Health locations use provider-based billing?
PBB will affect services offered by Phelps Health in these locations:
- Phelps Health Family Medicine – Rolla
- Phelps Health – St. James
- Phelps Health – Salem
- Phelps Health Waynesville Medical Plaza
- Phelps Health Walk-In Clinic – Rolla
- Phelps Health Walk-In Clinic – Waynesville
- Phelps Health Bond Building (both upper and lower levels)
- Phelps Health Pulmonology – Medical Office Building, Suite 550
- Phelps Health Women’s Health and Maternity Services – Medical Office Building, Suites 510 and 530
- Phelps Health Internal Medicine – Medical Office Building, Suite 350
- Phelps Health Pediatrics – Medical Office Building, Suite 300
- Phelps Health ENT and Allergy – Medical Office Building, Suite 300
- Phelps Health Physical Medicine and Rehabilitation – Medical Office Building, Suite 450
- Phelps Health Orthopedics and Podiatry – Medical Office Building, Suite 400
- Phelps Health Nephrology – Medical Office Building, Suite 480
- Phelps Health Urology – Medical Office Building, Suite 150
- Phelps Health Gastroenterology – Medical Office Building, Suite 580
- Phelps Health Heart and Vascular Center – Medical Office Building, Suite 500
- Phelps Health General Surgery – Delbert Day Cancer Institute, Second Floor
- Phelps Health Delbert Day Cancer Institute – Medical Oncology
- Phelps Health Delbert Day Cancer Institute – Radiation Oncology
- Phelps Health Senior Care – Medical Office Building, Suite 380
Why is Phelps Health changing to PBB?
Provider-based billing has become a common model of practice for health systems locally and around the US. This change will ultimately ensure that Phelps Health Hospital and clinics continue to provide safe and high-quality patient care.
This change benefits patients because all departments and clinics of the hospital are subject to strict quality standards and are monitored by The Joint Commission, an independent, not-for-profit organization that accredits and certifies more than 21,000 healthcare organizations and programs in the US.
In addition, the Centers for Medicare and Medicaid Services (CMS) have distinct payment programs for PBB and require that healthcare systems make it clear to the public which practices are part of the hospital.
View Example Billing Statement
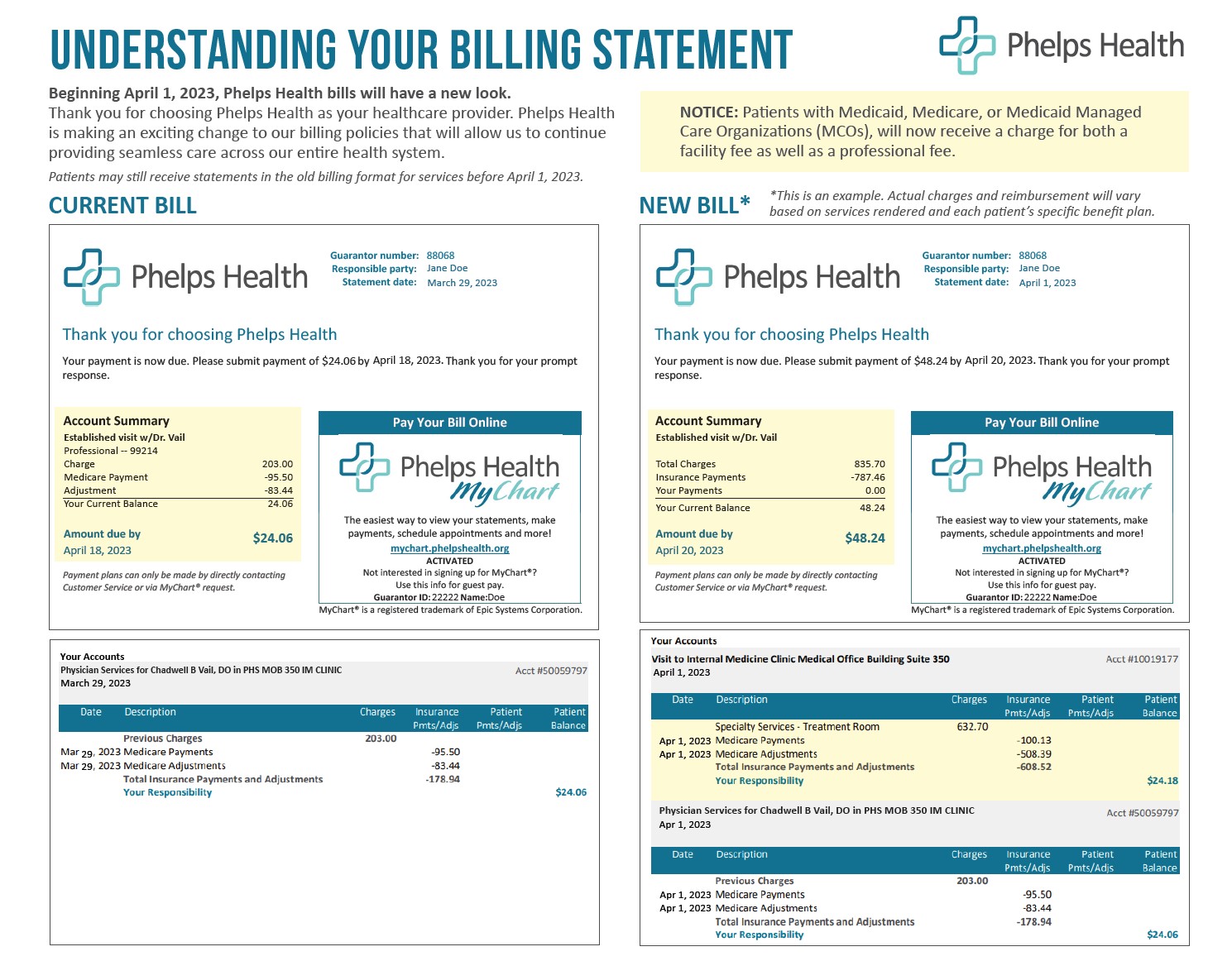
How will my bill change with PBB?
The PBB model will only affect patients with Medicaid, Medicare or Medicaid Managed Care Organizations (MCOs). At this time, PBB will not affect patients with commercial insurance (employer-offered insurance plans).
With PBB, visits to provider-based clinics will result in two charges to the patient: (1) a facility charge from the Hospital, and (2) a professional or physician charge for outpatient services and/or procedures. Previously, you may have seen all services and expenses in one single charge.
For patients with insurance, physician services will be processed under physician benefits, which are generally subject to patient copays. Hospital services will be processed under hospital benefits and subject to deductibles and coinsurance.
Will PBB affect my copays or deductibles?
Patients’ copays and deductibles at provider-based clinics will depend on their specific insurance benefits. Patients may have additional out-of-pocket expenses at provider-based clinics.
For most Medicare patients, the additional facility charge copay and deductible may add about $25 in out-of-pocket costs. However, the exact cost will vary depending upon services rendered and patients’ supplemental insurance coverage.
Medicare patients will incur a coinsurance cost to the hospital under PBB. Coinsurance and deductibles are generally covered by secondary insurance with Medicare. Patients should check their benefits or contact their health insurance company for details or questions.
Patients can visit https://phelpshealth.org/estimate-your-healthcare-cost, contact their provider’s office or call Phelps Health Patient Financial Services at (573) 458-7715 to request an estimate for services.
Will PBB change my appointments in any way?
You will continue to see your regular doctor and healthcare team to receive high-quality care. No changes will be made to scheduling appointments and tests.
Effective April 1, 2023, Medicare patients will be asked to complete a Medicare Secondary Payor Questionnaire (MSPQ) at each visit. We understand this will be repetitive, but this is a required regulation from CMS.
The goal of this questionnaire is to make sure that your bills are sent to Medicare or the appropriate agency responsible for paying them.
What should I ask my insurance carrier?
Making informed healthcare decisions is important. You may want to ask your insurance company the following:
- Does my benefit plan cover facility charges in a hospital-based outpatient clinic?
- How much of the charges are covered by my plan?
- Will the charges be applied to my deductible or subject to coinsurance?
What if I have questions about PBB or my bills?
As your healthcare provider, we are committed to helping you understand our financial and billing policies. For questions about PBB, including hospital and physician charges, call Phelps Health Patient Financial Services at (573) 458-7715.